What is Immune-Mediated Hemolytic Anemia (IMHA) in Dogs?
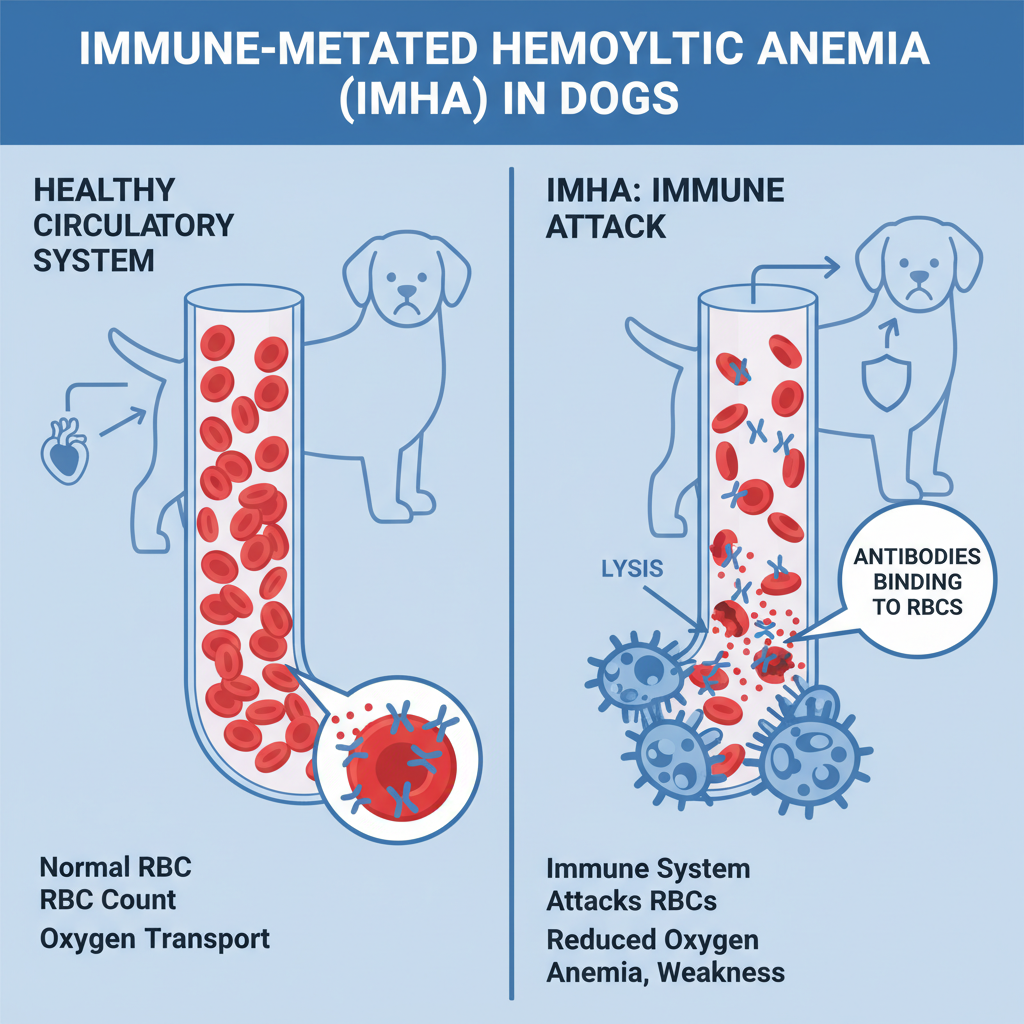
IMHA in dogs is a formidable health challenge, representing the most prevalent autoimmune disease encountered in canine companions. At its core, Immune-Mediated Hemolytic Anemia occurs when a dog’s own immune system mistakenly identifies its red blood cells (RBCs) as foreign invaders. In a cruel twist of biological fate, the body then launches an attack, forming antibodies that bind to and destroy these vital cells, ultimately leading to a severe deficiency known as anemia. This condition can manifest as either primary IMHA, where no specific underlying cause can be identified, or secondary IMHA, triggered by another underlying health issue. Regardless of its origin, the devastating outcome remains the same: the body turns against itself, dismantling the very cells essential for life.
Anemia itself signifies a critical shortage of red blood cells, hemoglobin, or both, within the bloodstream. Red blood cells serve as the tireless couriers, responsible for delivering life-sustaining oxygen to every tissue and organ throughout your dog’s body. Within these remarkable cells, hemoglobin— an iron-rich protein—is the molecular key that captures and transports oxygen.
When a dog becomes anemic, this crucial transport system falters. The dramatic reduction in RBCs and/or hemoglobin means a profound decrease in oxygen flow, jeopardizing the health and function of vital organs. This oxygen deprivation can rapidly escalate to organ damage and, tragically, even organ failure. Given its potential to become life-threatening with alarming speed, anemia is always a medical emergency. If you ever suspect your beloved dog is exhibiting signs of anemia, seeking immediate care at a local emergency veterinary hospital is absolutely paramount.
Recognizing the Symptoms of IMHA in Dogs
The clinical signs of IMHA in dogs can vary in severity but consistently point to a dog’s struggle with oxygen deprivation. Conscientious pet owners should be vigilant for any of the following indicators:
- Lethargy and profound lack of energy: Your dog may seem unusually tired, uninterested in play, or reluctant to move.
- Exercise intolerance: What was once a routine walk may now leave your dog winded and exhausted.
- Pale gums, often accompanied by a yellowish tint (jaundice): A healthy dog’s gums should be pink; paleness, especially with a yellow hue, is a critical warning sign. This yellowing can also be seen in the whites of the eyes or skin.
- Inappetence: A significant decrease in appetite or refusal to eat.
- Vomiting: Persistent or recurrent episodes.
- Dark orange to brown urine: This indicates the presence of broken-down red blood cells.
- Shortness of breath or rapid breathing: Even when at rest, your dog may be breathing faster or with more effort.
- Increased heart rate: The heart works harder to compensate for the lack of oxygen-carrying cells.
- Weakness or collapse: In severe cases, dogs may appear unsteady on their feet or completely lose consciousness.
Understanding the Causes of IMHA in Dogs
The journey to diagnosing the cause of IMHA in dogs often leads to two primary paths: primary or secondary. Primary IMHA remains a medical enigma, often described as idiopathic, meaning its cause is unknown. In these instances, a dog’s immune system, for reasons yet undiscovered, simply begins to attack its own red blood cells as if waking up one day with a misguided mission. Approximately 75% of canine IMHA cases fall into this category. It can manifest independently or in conjunction with other autoimmune conditions.
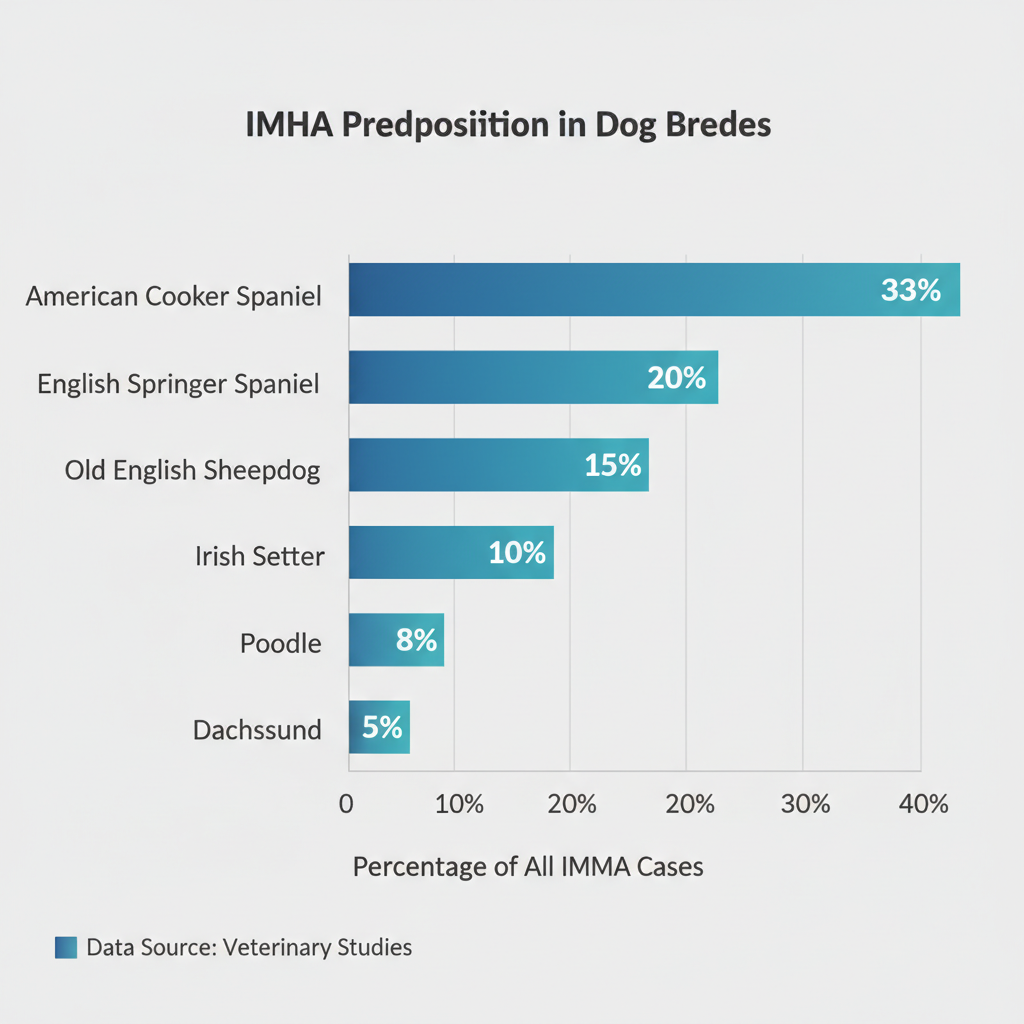
While the exact trigger for primary IMHA remains elusive, a genetic component is suspected in certain breeds. Veterinary professionals at Petscarelab, alongside leading industry researchers, have identified several breeds with a notable predisposition to IMHA:
- American Cocker Spaniel (accounting for a significant 33% of all cases)
- English Springer Spaniel
- Old English Sheepdog
- Irish Setter
- Poodle
- Dachshund
Secondary IMHA, conversely, arises when the body’s immune system turns on its red blood cells in response to an identifiable underlying health issue or external trigger. Common catalysts for secondary IMHA include:
- Infections:
- Parasitic: Such as various tick-borne diseases, including Ehrlichia, Anaplasma, Mycoplasma, and Babesia.
- Viral: Chronic persistent upper respiratory or gastrointestinal viruses.
- Bacterial: Leptospira, as well as various other acute and chronic bacterial infections.
- Neoplasia (Cancer):
- Any form of cancer can potentially disrupt immune regulation and trigger IMHA.
- Inflammatory Conditions:
- Broadly, any inflammatory process within the body has the potential to overstimulate the immune system, inadvertently triggering an autoimmune response like IMHA.
- Certain Drugs:
- Vaccines (in rare cases)
- Non-steroidal anti-inflammatory drugs (NSAIDs)
- Sulfonamides
- Penicillin and Cephalosporins
- Toxins:
- Bee stings
- Snake bites
- Zinc
- Onions and garlic
How Veterinarians Diagnose IMHA in Dogs
When a pet owner seeks veterinary attention for a dog displaying potential signs of anemia, a thorough physical examination is the first step. Our experienced veterinary professionals may initially suspect anemia based on findings such as pale or yellowish gums, skin, and eyes. However, the definitive diagnosis of anemia requires a complete blood count (CBC), a crucial diagnostic tool. If anemia is confirmed, further in-house blood tests will be performed to ascertain if Immune-Mediated Hemolytic Anemia is the underlying cause.
Based on the immediate results of these in-house diagnostics, your veterinarian will likely initiate a preliminary treatment plan to stabilize your pet. Concurrently, additional confirmatory tests will typically be sent to an external veterinary laboratory. You might hear terms like “Coombs test,“ “CBC with pathology review,“ and “reticulocyte count”—each designed to provide comprehensive details about the nature of the anemia and confirm the immune-mediated component. Additionally, baseline serum chemistry, which assesses organ function, and urinalysis will be performed to gain a broader picture of your dog’s overall health.
The subsequent phase of diagnostic testing is critical for screening your pet for any secondary causes of IMHA. This comprehensive screening often involves chest X-rays, an abdominal ultrasound, and specific infectious disease testing to uncover any hidden triggers for the immune response.
Treatment of IMHA in Dogs
While IMHA in dogs is a challenging and often life-threatening condition that cannot be “cured” in the traditional sense, it can frequently be driven into remission and successfully managed, allowing many dogs to lead fulfilling lives. Nevertheless, its severity almost always necessitates hospitalization and aggressive, multi-faceted therapy.
In rare instances, anemia may be detected very early during routine bloodwork screenings. In such fortunate cases, IMHA might be identified in its nascent stages, allowing for initial management with medications on an outpatient basis. However, the vast majority of IMHA cases demand immediate hospitalization for intensive care, including intravenous (IV) fluids and, critically, blood transfusions. The primary objective of blood transfusions is to stabilize your pet, providing immediate support while other treatments and medications are given time to take effect. It is not uncommon for severely affected dogs to require multiple transfusions to reach a stable state.
The cornerstone of IMHA treatment revolves around powerful immunosuppressive therapy. In the short term, this is typically achieved with high doses of corticosteroids, such as prednisone, to rapidly suppress the immune system’s destructive activity. Simultaneously, long-term immunosuppressive medications like mycophenolate, cyclosporine, and azathioprine are often introduced to provide sustained control.
If a diagnosis of secondary IMHA is made, additional therapies, such as antibiotics for an underlying infection, will be tailored specifically to treat the identified trigger. Anticoagulant therapy, often involving medications like clopidogrel (Plavix), may also be recommended to prevent dangerous blood clot formation, a potential complication of IMHA.
Given the complex nature of IMHA cases, our veterinary team will craft a highly individualized treatment plan specifically for your dog. In many instances, we may consult with or refer you to a veterinary internal medicine specialist to ensure the most advanced and comprehensive care.
Recovery and Management of IMHA in Dogs
Achieving successful outcomes for dogs battling IMHA in dogs hinges significantly on early diagnosis and the swift implementation of aggressive therapy. Even with the most dedicated medical intervention, the journey can be arduous, with approximately 50% of IMHA patients surviving long enough to be discharged from the hospital.
Most dogs recovering from IMHA will require an intensive hospital stay, typically lasting 2-7 days, within a 24-hour veterinary emergency facility. During this critical period, they receive continuous monitoring and treatments, including blood transfusions, to stabilize their condition.
Once your dog is released from the hospital, the commitment to their ongoing health continues. Regular recheck appointments with their internal medicine specialist or primary veterinarian are essential to closely monitor their red blood cell count and overall progress. Over several months, the high-dose prednisone is meticulously and gradually tapered down and eventually discontinued. However, long-term immunosuppressive medication(s) may need to be continued indefinitely to prevent relapse and maintain remission.
It is crucial to understand that IMHA is never truly “cured,” but with unwavering adherence to follow-up appointments and medication schedules, it can be successfully managed, allowing your dog to regain a good quality of life. While remission is the goal, relapse rates range from 11-15%, underscoring the need for vigilance.
It is vitally important to inform any new veterinary professionals about your dog’s history of IMHA, even if they are currently in remission. Maintaining a comprehensive chart of all current medications your dog is taking is also a wise practice. Future medications, evolving medical conditions, or even certain vaccines have the potential to inadvertently overstimulate the immune system of a dog with a previous autoimmune condition, thereby risking a relapse. Our dedicated veterinary team at Petscarelab will partner with you every step of the way to manage your dog’s complex long-term needs, ensuring they receive the best possible care for a full and happy life.







